MONTPELIER – The Vermont Department of Mental Health’s new budget includes funds for a “Peer Supports Credentialing Program.”
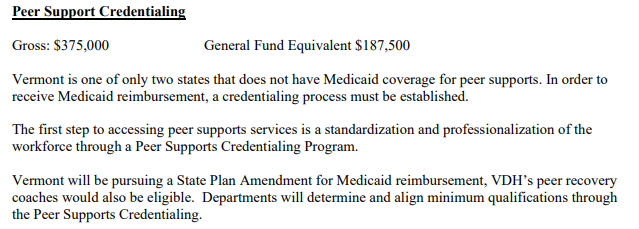
DMH requested an allocation of $187,500 from the state’s general fund to cover half of the projected cost of its startup and its first year of operations, based on the expectation that federal Medicaid dollars would pay for the remainder.
“The bulk of that money would actually go towards training,” Director of Adult Services Patricia Singer told the House Committee on Health Care. “We hope to train up to 60 folks in the first year.”
According to Singer, the program will target adult mental health peers exclusively, despite “some overlap” between their work and that of peer recovery coaches, who offer support for substance use conditions.
MadFreedom founder Wilda White, who testified alongside Singer, noted that the budget would support “the very basics of a certification program,” which she envisioned would someday offer additional credentials for mental health subspecialties such as geriatric support, forensic support, and peer supervision.
“That’s a ways off,” White predicted.
Most U.S. states have already established official certification processes for peers, which can make their services eligible for Medicaid reimbursement. Last year, after Vermont’s legislature failed to pass a bill to implement such a system, DMH – with the urging of the peerled organizations who’d drafted the legislation – determined to proceed through internal rulemaking
First, the department issued a $30,000 grant to Pathways Vermont’s Peer Workforce Development Initiative, which subcontracted Wilda White Consulting to host stakeholder meetings for a potential certification program. This spring, White completed a report with recommendations for DMH.
DMH does not have a specific timeline for a decision to accept or reject those recommendations, according to Deputy Commissioner Allison Krompf.
White’s report distinguishes between “assessment-based” and “professional” certification programs. The former would certify peers on the basis of their performance during a training period, while the latter would require an additional body to administer a test following the training. According to the report, the input received by White over the course of six public sessions, which 77 individuals attended, demonstrated a consensus in favor of a professional program.
The report calls for DMH to contract a peer-run organization for each of three central tasks: to screen candidates for eligibility to enroll in peer support training (on the basis, for instance, of testimony of “lived experience”); to develop and administer a training curriculum; and, in tandem with the Office of Professional Regulation, to issue credentials. A single vendor would handle the training statewide and could potentially take on the contract for screening as well. The endorsed screening standards would not disqualify applicants on the basis of their education or their state of residence. A criminal history would not bar them automatically.
The report also includes a draft of a Medicaid state plan amendment. Peer supporters employed by Medicaid-enrolled providers would practice under its guidelines, serving clients “who have a mental health or substance use condition and who have peer support included as a component of their person-centered, wellness plan, which serves as the plan of care.”
Once DMH has affirmed or rejected the report’s policy recommendations, the Peer Workforce Development Initiative will move on to what it calls “phase two” of its “work plan,” which will include helping to draft requests for proposals from peer-run entities for DMH’s possible use.