Nine years after Vermont legalized medical aid in dying through Act 39, the General Assembly updated the statute to permit physicians in virtual care settings to write prescriptions for life-ending medication for terminally ill patients.
“When we passed this law, telemedicine was an idea,” Sen. Dick McCormack, the bill’s lead sponsor, explained. “Telemedicine is now frequently used.”
S. 74 took effect immediately upon its passage this spring. In McCormack’s words, doctors “still have the option, upon an electronic communication, of saying, ‘I think I need to see you in person.’ But this makes the law under Act 39 consistent with usual medical practice, which is that the doctor would decide whether or not telemedicine is acceptable.”
The change does not eliminate the requirement for in-person verification of a terminal condition by way of a physical examination. But now, the doctor writing the prescription through an online consultation can rely on medical records attesting to such an examination having taken place previously, instead of having to administer one.
According to advocates, people with end-stage diseases often struggle to travel to medical appointments. They highlighted what they saw as an imperative to make end-of-life choice available to housebound patients.
“Most patients have very clear thoughts and wishes for how their life comes to an end, but they don’t have the energy or the emotional capacity to focus on that early, and so it’s often later in the illness, when people have a high symptom burden and their disease is quite advanced and their energy is quite low and time is quite short, that suddenly plans for the end of life are needed,” Dr. Diana Barnard, a palliative care physician at Porter Medical Center, described before the House Committee on Human Services.
Besides Vermont, nine states and Washington, D.C., have legalized assisted suicide. Testimony submitted by the Death with Dignity Political Fund in March asserted that, of these, Vermont was the only one that still did not permit the use of telemedicine for aid in dying.
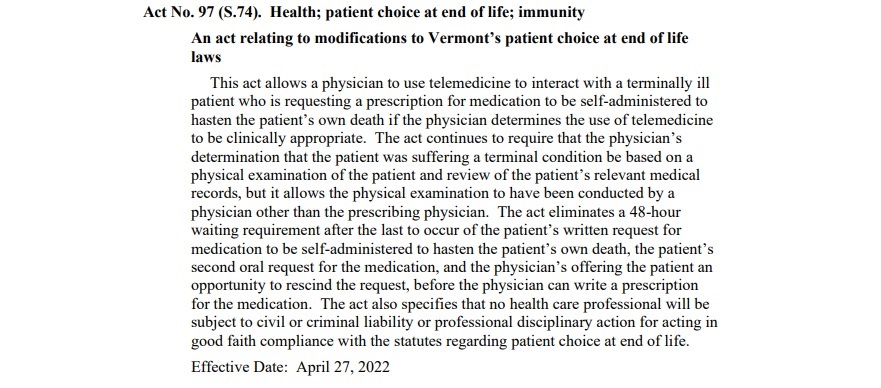
S.74 makes two other significant revisions to Act 39. One is to eliminate a 48-hour delay before the issuance of a prescription, following a still extant process of 15 days or more during which the patient submits and confirms their wish for a physician-assisted suicide.
By the account of Kim Callinan, president of the advocacy group Compassion & Choices, Vermont’s 17-day waiting period was the second-longest in the nation after Hawaii’s. At 15 days, Vermont “will still have one of the longer time frames in place, but it will be far more manageable for terminally ill people,” she said.
Finally, S.74 expands an immunity provision for doctors “acting in good faith compliance” with Act 39 to include all healthcare providers who may aid in an assisted suicide, such as nurses and pharmacists. Pharmacist Steve Hochtenberg told legislators that liability concerns had dissuaded some of his peers from filling prescriptions for life-ending medication.
Data reported by the Department of Mental Health shows that 116 Vermonters received medical aid in dying between May 31, 2013, and June 30, 2021. Cancer patients accounted for 77% of the total.
Act 39 continues to kindle debate. For its many of its proponents, the legalization of assisted suicide represents a triumph for patient-led care at medicine’s most crucial juncture, while its critics fear that the patient’s power to choose death over continued suffering could instead – despite various safeguards in the legislation – fall into the hands of a third party. This could be a family member or a doctor.
The Vermont Center for Independent Living’s executive director, Sarah Launderville, protested S.74’s expanded immunity clause for its “implicit trust” of the medical community. She alleged bias among providers who “advise against life-sustaining treatment for people with disabilities whose conditions would be treated were they not living with a disability.” Launderville advocated unsuccessfully for a provision requiring the collection of demographic data for Act 39 patients.
On April 13, Rep. Anne Donahue, who had opposed Act 39, proposed an amendment to S.74 intended to limit the risk of coercion in end-of-life choices. She argued that an exclusively virtual care environment would render manifestations of outside influence upon patients less visible to doctors.
“I believe it affects their ability to assess voluntariness – not being face to face; not being able to look in the eyes, because we can’t do that on Zoom; not being able to see who else might be in the room,” Donahue opined.
The amendment sought to mandate, during the assisted suicide request, one point of real-world contact with the patient by a healthcare provider, who could thereby attest to the patient’s independence. The provider wouldn’t have to be the doctor in charge of writing the prescription or a doctor at all. Donahue explained, by way of example, that the physical presence of a home health aide or a physical therapist, at any of five designated points within the patient’s 15-day application process for life-ending medication, would fulfill the requirement.
The House rejected the amendment on a vote of 41 to 98. Without it, the bill became law two weeks later.