BURLINGTON – The Department of Mental Health is actively looking to relieve Vermont’s overburdened emergency departments by expanding other options for care during mental health crises. There has not yet been any direct involvement by psychiatric survivors about specific criteria that should be included.
The Howard Center, Chittenden County’s community mental health center, has one idea.
It has already been under development and a spokesperson said it would be seeking broader input, but not until its proposal is further along.
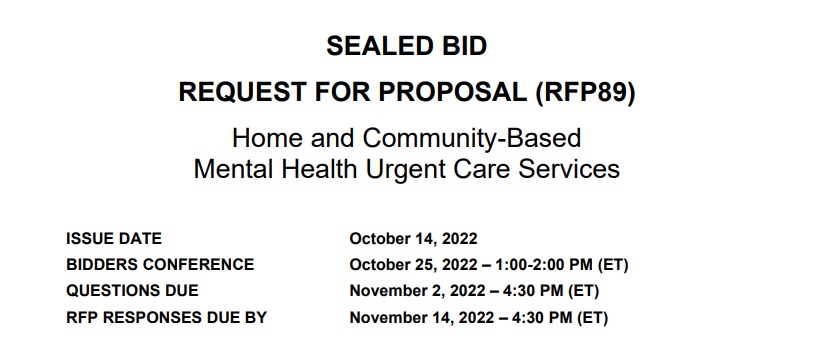
DMH issued a request for proposals for new urgent care services from qualified Medicaid providers in October. The document listed four potential models: a hospital-based “EmPATH” program (Emergency Psychiatric Assessment, Treatment & Healing); a “Living Room”-style crisis center with peer support; a “PUC” (Psychiatric Urgent Care) clinic; and a “CAHOOTS” (Crisis Assistance Health Out On The Streets) mobile response team.
There was no requirement for those who submit proposals in response to DMH to solicit input from the survivor community about their intended urgent care model.
Furthermore, the request for proposals appears to bypass the efforts of peer groups to develop peer respite programs that might provide crisis support options in similar ways.
Last year, the effort by four peer-affiliated organizations to propose that model failed to gain funding by the legislature. DMH said that the new programs described by the RFP were all based on a special federal funding opportunity, so they can only be developed by organizations that can receive Medicaid funds.
“Peer respites are not eligible for enhanced funding because services are not billable to Medicaid,” DMH said. Peer support staff are not certified in Vermont, which is a barrier to that funding.
Before the RFP’s release, the Howard Center had already begun working to develop a plan for an urgent care clinic for mental health needs in Burlington. Initial conversations included potential partnerships with the University of Vermont Medical Center and the Community Health Center of Burlington.
According to Howard Center Chief Client Services Officer Catherine Simonson, it would operate much like an urgent care clinic for physical injuries and illnesses. “For instance, if you sprain your ankle,” Simonson said, “that doesn’t necessarily mean you have to go to the emergency department, but you need attention. You can’t wait till your doctor’s office opens up.”
The clinic would be open to the public, with no appointments needed, for about 12 hours a day. Clients would not be able to stay overnight, but Simonson envisions that those in need of additional stabilization would return the next day for a follow-up.
The Howard Center aims to find a communitybased site for the program in the vicinity of UVMMC, which would allow staff to easily refer patients to the emergency department if they meet criteria for hospitalization.
“Right now, for Howard Center, we don’t have a building set up such that there’s a lot of space for walk-ins,” Simonson observed.
The Howard Center already has a mobile response team for mental health emergencies, but Simonson believes that a brick-and-mortar clinic would provide a valuable supplement.
“It’s recognizing that many people in our community are choosing either not to wait for mobile outreach, or they want a place to go,” she said. “They don’t want somebody coming to their home or to wherever they are.”
DMH initially took part in discussions about the idea with the Howard Center and its partners but later assumed the role of a neutral party as it prepared to evaluate responses to the request for proposals. “Once an RFP is issued, they can’t be a part of any planning,” Simonson noted.
Pathways Vermont, Burlington’s peerled specialized service agency, joined later conversations. In Simonson’s vision, peers from Pathways and from the Howard Center’s own peer support team would join mental health clinicians, crisis workers, case managers, administrative staff, and a medical provider in a “multidisciplinary approach.”
“Our hope with the urgent care center is that it will be staffed such that people are not having to wait a long time to get their needs met and to be able to see somebody,” Simonson added.
Patients, she said, would enjoy a “calmer, trauma-informed” environment with “a little bit more personal space” than they’d find in an ED.
Simonson pledged that the Howard Center would solicit broader input on the plan upon securing a location and a contract with DMH. This would include consulting the Howard’s Center Community Advocacy Network Standing Committee and holding forums “for folks who identify as psychiatric survivors and other groups.”
“The fact that we haven’t done it yet is not so much not seeing the value in that, but feeling like we need to be further along, because there’s still a lot of work to be done,” Simonson explained.
DMH’s deadline for proposals was Nov. 14.